Fibrocartilaginous Infarction:
Even though animals do not suffer from to the same degree of vascular disease as human
beings, infarction of the spinal cord with fibrocartilaginous material is not uncommon.
It occurs in
any breed of dogs, but is most common in large breeds, such as Great Danes, Labrador retrievers
and German Shepherds. Although both arteries and veins can be affected, most commonly it is the
venous system of the spinal cord which is obstructed, leading to a hemorrhagic infarction.
It is
believed that herniation of the nucleus pulposus takes place either into the vertebral body or the
venous sinuses within the spinal column. Since the vertebral body represents a vascular space
communicating with the spinal venous system, the material gains access to the spinal veins. These veins do not have valves, allowing the fibrocartilaginous material to flow up and down the spinal
column. When intra-thoracic pressure increases, this material can be back-flushed into small
penetrating spinal cord veins. When the intra-thoracic pressure returns to normal, the veins collapse
trapping the material and leading to excessive venous pressure upstream to the occlusion. The
venules rupture leading to a hemorrhagic infarction.
The pattern of infarction usually affects a
quadrant of the spinal cord, although initial signs may affect more of the spinal pathways from
inflammation and spinal cord swelling.
The infarction can occur anywhere along the spinal cord,
but the causal cervical and mid- to lower lumbar spinal cord segments appear to be most frequently
involved.
The presence of spinal cord infarction should be suspected whenever a patient presents with
acute onset of paresis or paralysis which is markedly asymmetrical and there is no evidence of
hyperpathia.
Vascular disease is generally acute and non-progressive. In addition, the spinal cord
contains pain pathways, but no pain receptors. As such, strict diseases within the spinal cord
without meningeal involvement are usually not painful. Most of the other diagnostic tests will be
within normal limits.
Occasionally, there will be evidence of hemorrhage on CSF analysis. Spinal
radiographs, do not demonstrate the disease, but may reveal other evidence of spinal column
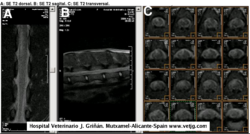
degeneration. Myelography will be normal or demonstrate mild intramedullary swelling. In a small
number of cases (where the vascular occlusion is secondary to a systemic disease), the minimum
data base will show evidence of the systemic disease.
The treatment of spinal cord infarction is that for acute spinal cord injury, using
methylprednisolone at 30 mg/kg initially. This is followed by 15 mg/kg every 8 hours for the first
24-48 hours. Then, oral prednisolone is begun at 0.5 mg /kg every 12 hours for 5 days. I continue
prednisolone at 0.5 mg/kg every other day, in the morning, for up to another 2 weeks.
Many cases
will improve dramatically within the first week, although they will still improve over several
months. If there has been no improvement in the first week, re-examination and additional tests may
be indicated. Since usually only a quadrant of the spinal cord is affected, the patient will improve
most on the unaffected side. Reorganization will usually allow these patients to function adequately.
Spinal cord infarction from fibrocartilaginous material is a sporadic problem and, usually, does not
reoccur.
|